Alberta’s medical laboratories have gone from public, to private, and back to public in less than one year. What has this back and forth action cost Albertans? This and other questions are explored in this CBC report.
Alberta’s medical laboratories have gone from public, to private, and back to public in less than one year. What has this back and forth action cost Albertans? This and other questions are explored in this CBC report.
Martha’s Rule is a new policy that aims to give patients and the patient’s families greater voice in the the care their loved one is receiving without the fear of retribution or the like. Had this rule existed in 2021, perhaps Martha’s outcome would have been very different.
As Martha’s mother said, “‘I desperately wish that I’d felt able, with no fear of being the target of ill-temper or condescension, to ask for a second opinion from outside the liver team when I became concerned about Martha’s deterioration.’”
Click here to read about Martha’s Rule.
Oft times, the shortest tweets say the most.
Doctors still don't get how traumatizing it can be for patients to not be believed.
— Steven Phillips, MD (@StevePhillipsMD) January 13, 2023
When you receive a serious health diagnosis one of the first things that comes to mind is, “Am I going to die?”. Sometimes we are fortunate and hear the doctor’s reply, “No”, but there is usually a “but” associated with that and that “but” often means something like surgery or treatments of some type. Other times we do hear, “Yes” and it may be soon or may be sometime in the future.
I was diagnosed with early-stage bladder cancer in September 2008. When my urologist gave me the results of the biopsy by phone about two weeks after my surgery to remove the bladder tumours, like many people my brain shut down the minute that he used the “C” word. Prior to his call, I had been hoping against all hope that there would be that last minute miracle and I would get the good news that the tumours were benign. That was not in my fortune cards. My official diagnosis in medicalese was “early-stage non-muscle invasive high grade transitional cell urothelial carcinoma.” I will tell you those words sounded ominous to say the least. So how close was I to dying and potentially leaving my husband with two underage sons to raise on his own?
My urologist explained that my diagnosis was a “good news” “bad news” scenario but most likely more good news. The good news part was that it was early stage hence the term “non-muscle invasive” meaning that the cancer was on the inner surface of the bladder wall It had not invaded the inner layers. The not so good news was that the cancer was high-grade meaning aggressive and with some risk of progression should it recur.
To reduce the risk of recurrence and progression he recommended immunotherapy treatments, which involved a drug called BCG or Bacillus Callumette Guerin. The drug is inserted into the bladder via a urinary catheter, and you hold the drug inside for about 2 hours and then void it out. The protocol called for a treatment once a week for six weeks and then after about a month, I would see him for a follow-up cystoscopy exam (camera inserted into the bladder via the urethra) to check to see how things were. The way he explained it, it sounded simple enough, but my mind went in a million directions all at once. I did ask about risks of the treatment, but he made it sound like a breeze compared to the traditional systemic chemotherapy that many other cancer patients receive. My brain was too frozen at the time to ask any more questions, plus I could sense that my doctor was really busy, (are they ever anything else?) and needed to get off the phone. He finished the call by telling me that his receptionist would be in touch once the treatments were booked.
Once off the phone, the brain numbness started to wear off and my thought was, “What just happened here?” It was too much. I just started to bawl. Thankfully my hubby was at work and the kids were still at school. It gave me some time to get my head together.
Truth be told, I was terrified of the idea of those treatments. While it was not chemo, I knew that it was a powerful drug from the description that my doctor had given me. I knew people that had died from complications of chemotherapy treatments. My urologist told me that most people that did the treatments just felt like they had a good dose of the flu for a couple of days afterwards. So, exactly how right would he be?
As it turned out, he was right to some degree. What he didn’t realize though was that I was a fifty-year-old woman just entering menopause. The BCG made the hot flashes and night sweats far worse than they would have normally been. So, I had menopause symptoms on top of BCG side effects – fun stuff. And when I asked about HRT to relieve the symptoms, I was told that it was not advisable to combine that with cancer treatment. Oh, and I did have some side effects that many cancer patients receiving chemo have – chemo brain that affects concentration and memory, digestive issues and a whole lot of fatigue. Thankfully hair loss was not one of them.
I powered through and after the six weeks of treatments were finished, I got good news at my follow-up checkup. No tumours. My doctor was very pleased and told me that all I needed to do now was come for a cystoscopy check every three months. If I remained clear of bladder cancer for two years, I would graduate to check ups every six months. This checkup happened right before Christmas 2008. At the conclusion of my exam, he wished me Merry Christmas. It was the best Christmas gift I have ever received. My hope was restored, and I felt like I had a future. I would get to see my boys grow up after all.
I nearly made it to the two-year clear mark when a single tumour of the same type, stage and grade was found on the top of my bladder in July 2010. I had been so hopeful that I’d make it to the two-year mark (Christmas 2010) because I had been doing so well. I hadn’t even had a cold. Well, after viewing that tumour on the monitor, my hopes were more than dashed. I was devastated and felt hope for my future sinking fast. What now?
Well, I had another surgery to remove the tumour and that was followed by another set of six treatments which were followed by three sets of three at three, six and twelve months after the set of the six. This was my life for the next eighteen months. The side effects were cumulative and by the end of it all, I was feeling pretty crummy. It would be more than a year before I started feeling close to normal.
I had suffered some pretty serious depression with the first go round especially because I had no one to talk to. What I really needed was to talk to another woman who was going through the same thing. Back then there were not the resources for this as there are now. I did not want to go down the deep dark rabbit hole like the first time. Somewhere, somehow, someone had to give me hope.
By this time, I had learned how to use the computer better and decided to google support for bladder cancer. The link for Bladder Cancer Canada popped up. Realizing it was a Canadian organization made me curious. I went on their website. As I perused all the information on the different links, I also discovered a discussion forum. From here I was able to connect with both men and women of all stripes and various journeys with bladder cancer. They helped me put my situation into a better perspective. After this, I was able to understand that while serious, my situation was not life threatening and that restored my hope that I was going to be okay.
Partially through communicating with others and my own personal reading, I learned more about eating a better diet, the importance of exercise, correct use of vitamins and supplements and most important of all – improving my mindset.
Before my cancer diagnosis, I was turning into a really negative person. I’d been through a lot during the past decade or so, and it was getting to the point that I’d reached burnout. Getting cancer was a real wakeup call and made me question everything: who I was, how I got to where I was, what kind of changes that I needed to make and where I should go from here. In other words, a potentially life-threatening diagnosis made me into a better person and gave me hope for the future.
As the months of “all clear” progressed to years, I realized the gift that I’d been given. I have had a second chance. A chance to do good, a chance to live better and best of all hope for tomorrow.

For more information on Bladder Cancer go to www.bladdercancercanada.org
I’ve been a gardener most of my life. The three people that instilled this love of growing things in me were my mother and godfather and a former next door neighbor who Mom was good friends with. Mom was mostly into growing flowers in and outside of the house. My godfather grew roses (which he won awards for) and had an extensive vegetable garden. Mrs. V. the next door neighbor, could grow anything. She grew all kinds of flowers and some veggies.
While many of the techniques and knowledge that I gained from them helped me along my gardening path, I had to learn a lot of new stuff when I moved to Calgary. The climate is much colder in the wintertime and much more variable in the warmer months. The fickleness of springtime can sometimes lead to a total loss of one’s potential seasonal crops if they are caught in a cold and/or unseasonable spring.
The two times in my life that gardening has proven to be a real sanity saver are when I was diagnosed with cancer in 2008 and in 2020 when the world faced the Covid 19 pandemic. Gardening during these times gave me a sense of control when all seemed out of control. Feeling the energy from the ground as I sat or kneeled when I planted the seeds calmed me. The warmth from the sun on my head and shoulders massaged me in no way that any masseuse could.
With both times my ability to travel was limited so I knew that I had to find things to do at home. Not being content with activities that didn’t have some kind of “work” element attached to them, I knew that gardening would help with that. The exercise from the physical work strengthens my muscles, the vitamin D from the sun boosts my mood better than any antidepressant ever could.
After a gardening session I often sit in my swing on the back deck with a cool drink and take in the scene around me. Just this afternoon I watched a mother sparrow and her not quite totally fledged little one land on my fence so that she could feed him/her. A mother robin with a worm in her beak paused on my fence on her way back to her nest. A grey squirrel chased a magpie while running along the top of a neighbour’s fence all the while screaming with a mouthful of food. A family of six young magpies who can now finally fly properly flit between the trees, squawking at each other. Their sibling spats usually involve food as their parents have now left them to fend for themselves.
After a rather raucous start in the spring with all the birds declaring their love for each other and staking out their claims for nesting sites, all is much quieter now because most of the birds are raising their young and want to keep them safe by not revealing the whereabouts of the nest.
In another month or so, my garden will start to produce in earnest, and I will be pressed to keep up with all the bounty by canning, freezing and pickling things. At the same time the last few fledglings will be learning to fly and the birds that normally are in the mountains will return. I notice the seasons change not only by my garden and the weather, but by the birds as well.
The garden and the birds were not affected by my cancer diagnosis nor by the covid 19 pandemic. Life for them goes on as the seasons change.


Date: Tuesday, Sept 27, 2022
Time: 11:30 – 4:30pm
Location: Red & White Club
McMahon Stadium
1833 Crowchild Trail NW
“As our population grows older, we are also seeing an influx of technologies designed to make our lives easier and keep us better connected. This half-day event, presented by the O’Brien Institute for Public Health Brenda Strafford Centre on Aging, the Canadian Frailty Network and AGE-WELL, will host leading researchers who are exploring how accessible and smart technologies are influencing our aging experiences. This free, public event will begin with a lunch and networking session, followed by an afternoon of interactive talks.”
Click here for more information.
It was a difficult decision for our family to share this story. My dad was a quiet, private person who didn't like the spotlight, and I worried about protecting his dignity while also making sure Albertans were told what is happening in our hospitals. https://t.co/7zo1kuIbL2
— Bridget Stirling (@bridgetstirling) July 29, 2022
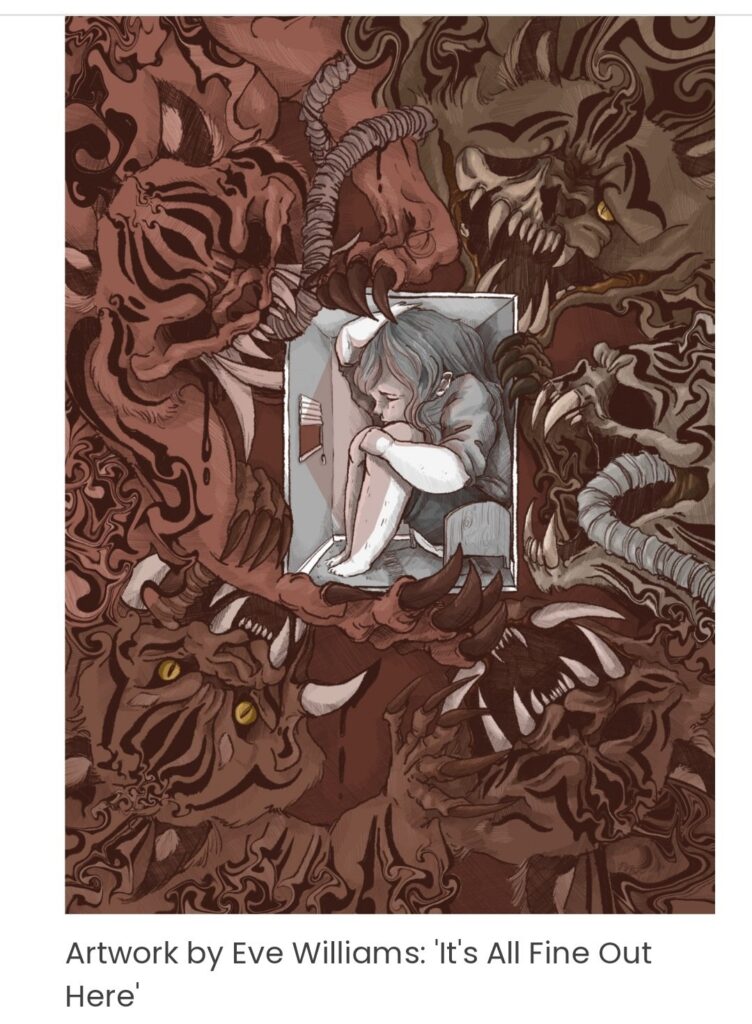
As greater emphasis is being placed on “getting on with life” or at the very least “learning to live with COVID-19” people who are immunocompromised, disabled or have medical issues that put them or those they care for at risk are being isolated, alienated, ostracized and ignored by much of society. In an article entitled, “Those who are Disabled and Immunocompromised need to be supported, not ignored,” Eva Williams describes this new reality. According to her, “The way that vulnerable people are currently being treated is nothing short of barbaric.” Click here to read Williams’ article.
Here is a Twitter thread that expresses what many people are feeling.
I am so mad. So Mad. Our #abhealth system is beyond broken. A dear friend and new mom is needing transfer from a rural hospital to #RDRHC for a procedure. A very necessary procedure to remove excess fluid around her lungs. 1/5
— Tired AB Nurse Blocked by Kenney (@tired_albertan) July 3, 2022

What does “patient safety” mean?
The University Health Network Open Lab team is working closely with the safety team at Healthcare Excellence Canada on their Defining Safety project. The goal of this project is to understand perspectives on the definition and future of patient safety from patients, caregivers, professionals, and leaders across Canada.
As a means of obtaining insights and ideas from Canadians, a ‘thought exchange’ about patient safety has been created. This exchange is a completely anonymous platform that provides space for participants to describe what they think the salient features are that should be included in a definition of patient safety.
If you live in Canada and want to join in the conversation on patient safety, click here.